Being older
Your risk of colorectal cancer goes up as you age. Younger adults can get it, but it is much more common after age 50.
A personal history of colorectal polyps or colorectal cancer
If you have a history of adenomatous polyps (adenomas), you are at increased risk of developing colorectal cancer. This is especially true if the polyps are large, if there are many of them, or if any of them show dysplasia.
If you have had colorectal cancer, even though it has been completely removed, you are more likely to develop new cancers in other areas of the colon and rectum. The chances of this happening are greater if you had your first colorectal cancer when you were younger.
A personal history of inflammatory bowel disease
If you have inflammatory bowel disease (IBD), including either ulcerative colitis or Crohn’s disease, your risk of colorectal cancer is increased.
IBD is a condition in which the colon is inflamed over a long period of time. People who have had IBD for many years, especially if untreated, often develop dysplasia. Dysplasia is a term used to describe cells in the lining of the colon or rectum that look abnormal, but are not true cancer cells. They can, however, change into cancer over time.
If you have IBD, you may need to start being screened for colorectal cancer when you are younger and be screened more frequently.
Inflammatory bowel disease is different from irritable bowel syndrome (IBS), which does not increase your risk for colorectal cancer.
A family history of colorectal cancer or adenomatous polyps
Most colorectal cancers are found in people without a family history of colorectal cancer. Still, as many as 1 in 5 people who develop colorectal cancer have other family members who have had it.
People with a history of colorectal cancer in a first-degree relative (parent, sibling, or child) are at increased risk. The risk is even higher if that relative was diagnosed with cancer when they were younger than 45, or if more than one first-degree relative is affected.
The reasons for the increased risk are not clear in all cases. Cancers can “run in the family” because of inherited genes, shared environmental factors, or some combination of these.
Most people with colorectal cancer have no family history of colorectal cancer. Still, as many as 1 in 5 people who develop colorectal cancer have other family members who have been affected by this disease.
Having family members who have had adenomatous polyps is also linked to a higher risk of colon cancer. (Adenomatous polyps are the kind of polyps that can become cancerous.)
If you have a family history of adenomatous polyps or colorectal cancer, talk with your doctor about the possible need to begin screening before age 50. If you have had adenomatous polyps or colorectal cancer, it’s important to tell your close relatives so that they can pass along that information to their doctors and start screening at the right age.
Having an inherited syndrome
About 5% to 10% of people who develop colorectal cancer have inherited gene changes (mutations) that can cause family cancer syndromes and lead to them getting the disease.
The most common inherited syndromes linked with colorectal cancers are familial adenomatous polyposis (FAP) and Lynch syndrome (hereditary non-polyposis colorectal cancer, or HNPCC), but other rarer syndromes can also increase colorectal cancer risk.
Familial adenomatous polyposis (FAP): FAP is caused by changes (mutations) in the APC gene that a person inherits from his or her parents. About 1% of all colorectal cancers are caused by FAP.
In the most common type of FAP, hundreds or thousands of polyps develop in a person’s colon and rectum, usually in their teens or early adulthood. Cancer usually develops in 1 or more of these polyps as early as age 20. By age 40, almost all people with FAP will have colon cancer if their colon hasn’t been removed to prevent it. People with FAP also have an increased risk for cancers of the stomach, small intestines, and some other organs.
- In attenuated FAP, which is a subtype of this disorder, patients have fewer polyps (less than 100), and colorectal cancer tends to occur at a later age.
- Gardner syndrome is a type of FAP that also has non-cancerous tumors of the skin, soft tissue, and bones.
Lynch syndrome (hereditary non-polyposis colon cancer, or HNPCC): Lynch syndrome accounts for about 2% to 4% of all colorectal cancers. In most cases, this disorder is caused by an inherited defect in either the MLH1 or MSH2 gene, but changes in other genes can also cause Lynch syndrome. These genes normally help repair DNA that has been damaged.
The cancers in this syndrome develop when people are relatively young. People with Lynch syndrome can have polyps, but they tend to only have a few, not hundreds as in FAP. The lifetime risk of colorectal cancer in people with this condition may be as high as 80%, but this depends on which gene is affected.
Women with this condition also have a very high risk of developing cancer of the endometrium (lining of the uterus). Other cancers linked with Lynch syndrome include cancer of the ovary, stomach, small intestine, pancreas, kidney, brain, ureters (tubes that carry urine from the kidneys to the bladder), and bile duct.
For more information on Lynch syndrome, see Do We Know What Causes Colorectal Cancer? and Can Colorectal Cancer Be Prevented? and Family Cancer Syndromes.
Turcot syndrome: This is a rare inherited condition in which people have a higher risk of adenomatous polyps and colorectal cancer, as well as brain tumors. There are actually 2 types of Turcot syndrome:
- One is caused by gene changes similar to those seen in FAP, in which cases the brain tumors are medulloblastomas.
- The other is caused by gene changes similar to those seen in Lynch syndrome, in which cases the brain tumors are glioblastomas.
Peutz-Jeghers syndrome: People with this inherited condition tend to have freckles around the mouth (and sometimes on their hands and feet) and a special type of polyp called hamartomas in their digestive tracts. These people are at a much higher risk for colorectal cancer, as well as other cancers, and they usually are diagnosed at a younger than usual age. This syndrome is caused by mutations in the STK11 (LKB1) gene.
MUTYH-associated polyposis: People with this syndrome develop colon polyps that will almost always become cancerous if the colon is not watched closely with regular colonoscopies. These people also have an increased risk of cancers of the small intestine, skin, ovary, and bladder. This syndrome is caused by mutations in the MUTYH gene (which is involved in “proofreading” the DNA to fix any mistakes) and often leads to cancer at a younger age.
Since many of these syndromes above are associated with colorectal cancer at a young age and also linked to other types of cancer, identifying families with these inherited syndromes is important. It lets doctors recommend specific steps such as screening and other preventive measures when the person is younger. Information on risk assessment, and genetic counseling and testing for these syndromes can be found in Genetic Testing, Screening, and Prevention for People with a Strong Family History of Colorectal Cancer.
Your racial and ethnic background
African Americans have the highest colorectal cancer incidence and mortality rates of all racial groups in the United States. The reasons for this are not yet understood.
Jews of Eastern European descent (Ashkenazi Jews) have one of the highest colorectal cancer risks of any ethnic group in the world.
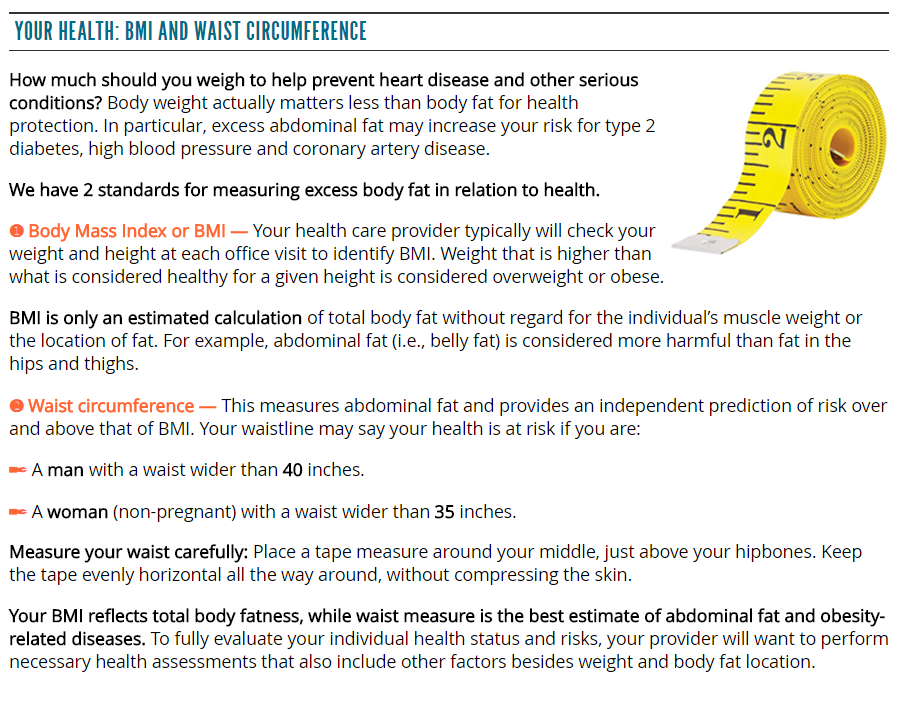
Having type 2 diabetes
People with type 2 (usually non-insulin dependent) diabetes have an increased risk of colorectal cancer. Both type 2 diabetes and colorectal cancer share some of the same risk factors (such as being overweight and physical inactivity). But even after taking these factors into account, people with type 2 diabetes still have an increased risk. They also tend to have a less favorable prognosis (outlook) after diagnosis.
Factors with unclear effects on colorectal cancer risk
Night shift work
Some studies suggest working a night shift regularly may increase the risk of colorectal cancer. It is thought this might be due to changes in levels of melatonin (a hormone that responds to changes in light) in the body. More research is needed.
Previous treatment for certain cancers
Some studies have found that men who survive testicular cancer seem to have a higher rate of colorectal cancer and some other cancers. This might be because of the treatments they have received such as radiation therapy.
Several studies have suggested that men who had radiation therapy to treat prostate cancer might have a higher risk of rectal cancer because the rectum receives some radiation during treatment. Most of these studies are based on men treated in the 1980s and 1990s, when radiation treatments were less precise than they are today. The effect of more modern radiation methods on rectal cancer risk is not clear.
https://www.cancer.org/cancer/colon-rectal-cancer/causes-risks-prevention/risk-factors.html
 Colorectal polyps and colorectal cancer don’t always cause symptoms, especially at first. Someone could have polyps or colorectal cancer and not know it. That is why getting screened regularly for colorectal cancer is so important.
Colorectal polyps and colorectal cancer don’t always cause symptoms, especially at first. Someone could have polyps or colorectal cancer and not know it. That is why getting screened regularly for colorectal cancer is so important.