There’s a ton of incredibly promising intermittent fasting (IF) research done on fat rats. They lose weight, their blood pressure, cholesterol, and blood sugars improve… but they’re rats. Studies in humans, almost across the board, have shown that IF is safe and incredibly effective, but really no more effective than any other diet. In addition, many people find it difficult to fast.But a growing body of research suggests that the timing of the fast is key, and can make IF a more realistic, sustainable, and effective approach for weight loss, as well as for diabetes prevention.
The backstory on intermittent fasting
IF as a weight loss approach has been around in various forms for ages, but was highly popularized in 2012 by BBC broadcast journalist Dr. Michael Mosley’s TV documentary Eat Fast, Live Longer and book The Fast Diet, followed by journalist Kate Harrison’s book The 5:2 Diet based on her own experience, and subsequently by Dr. Jason Fung’s 2016 bestseller The Obesity Code. IF generated a steady positive buzz as anecdotes of its effectiveness proliferated.
As a lifestyle-leaning research doctor, I needed to understand the science. The Obesity Codeseemed the most evidence-based summary resource, and I loved it. Fung successfully combines plenty of research, his clinical experience, and sensible nutrition advice, and also addresses the socioeconomic forces conspiring to make us fat. He is very clear that we should eat more fruits and veggies, fiber, healthy protein, and fats, and avoid sugar, refined grains, processed foods, and for God’s sake, stop snacking. Check, check, check, I agree. The only part that was still questionable in my mind was the intermittent fasting part.
Intermittent fasting can help weight loss
IF makes intuitive sense. The food we eat is broken down by enzymes in our gut and eventually ends up as molecules in our bloodstream. Carbohydrates, particularly sugars and refined grains (think white flours and rice), are quickly broken down into sugar, which our cells use for energy. If our cells don’t use it all, we store it in our fat cells as, well, fat. But sugar can only enter our cells with insulin, a hormone made in the pancreas. Insulin brings sugar into the fat cells and keeps it there.
Between meals, as long as we don’t snack, our insulin levels will go down and our fat cells can then release their stored sugar, to be used as energy. We lose weight if we let our insulin levels go down. The entire idea of IF is to allow the insulin levels to go down far enough and for long enough that we burn off our fat.
Intermittent fasting can be hard… but maybe it doesn’t have to be
Initial human studies that compared fasting every other day to eating less every day showed that both worked about equally for weight loss, though people struggled with the fasting days. So I had written off IF as no better or worse than simply eating less, only far more uncomfortable. My advice was to just stick with the sensible, plant-based, Mediterranean-style diet.
New research is suggesting that not all IF approaches are the same, and some are actually very reasonable, effective, and sustainable, especially when combined with a nutritious plant-based diet. So I’m prepared to take my lumps on this one (and even revise my prior post).
We have evolved to be in sync with the day/night cycle, i.e., a circadian rhythm. Our metabolism has adapted to daytime food, nighttime sleep. Nighttime eating is well associated with a higher risk of obesity, as well as diabetes.
Based on this, researchers from the University of Alabama conducted a study with a small group of obese men with prediabetes. They compared a form of intermittent fasting called “early time-restricted feeding,” where all meals were fit into an early eight-hour period of the day (7 am to 3 pm), or spread out over 12 hours (between 7 am and 7 pm). Both groups maintained their weight (did not gain or lose) but after five weeks, the eight-hours group had dramatically lower insulin levels and significantly improved insulin sensitivity, as well as significantly lower blood pressure. The best part? The eight-hours group also had significantly decreased appetite. They weren’t starving.
Just changing the timing of meals, by eating earlier in the day and extending the overnight fast, significantly benefited metabolism even in people who didn’t lose a single pound.
So is this as good as it sounds?
I was very curious about this, so I asked the opinion of metabolic expert Dr. Deborah Wexler, Director of the Massachusetts General Hospital Diabetes Center and associate professor at Harvard Medical School. Here is what she told me. “There is evidence to suggest that the circadian rhythm fasting approach, where meals are restricted to an eight to 10-hour period of the daytime, is effective,” she confirmed, though generally she recommends that people “use an eating approach that works for them and is sustainable to them.”
So here’s the deal. There is some good scientific evidence suggesting that circadian rhythm fasting, when combined with a healthy diet and lifestyle, can be a particularly effective approach to weight loss, especially for people at risk for diabetes. (However, people with advanced diabetes or who are on medications for diabetes, people with a history of eating disorders like anorexia and bulimia, and pregnant or breastfeeding women should not attempt intermittent fasting unless under the close supervision of a physician who can monitor them.)
4 ways to use this information for better health
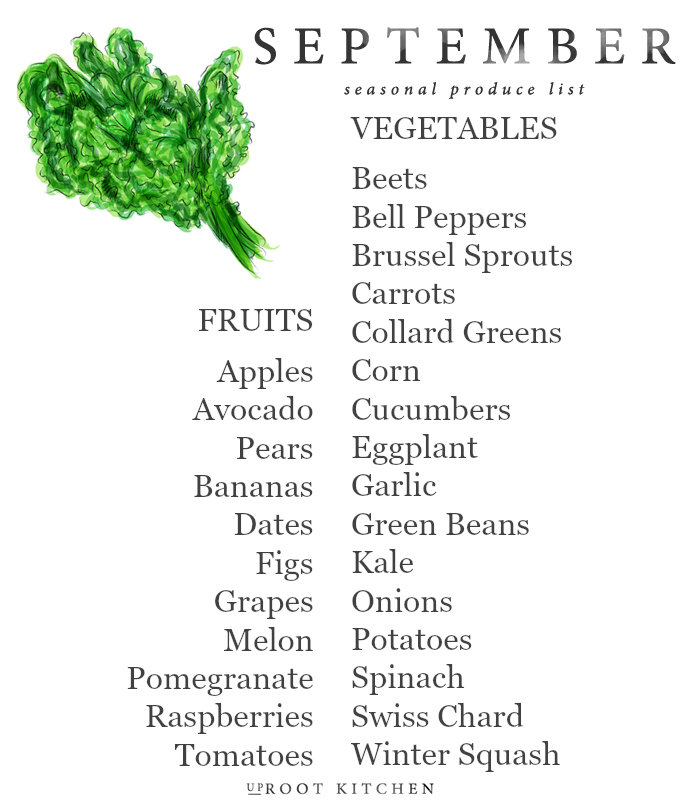
- Avoid sugars and refined grains. Instead, eat fruits, vegetables, beans, lentils, whole grains, lean proteins, and healthy fats (a sensible, plant-based, Mediterranean-style diet).
- Let your body burn fat between meals. Don’t snack. Be active throughout your day. Build muscle tone.
- Consider a simple form of intermittent fasting. Limit the hours of the day when you eat, and for best effect, make it earlier in the day (between 7 am to 3 pm, or even 10 am to 6 pm, but definitely not in the evening before bed).
- Avoid snacking or eating at nighttime, all the time.
.health.harvard.edu/blog/intermittent-fasting-surprising-update-2018062914156