
Payor Mix
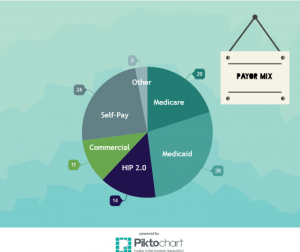
Based on 220 patients/Month:
Incident To: 99211 vs. Facility Fee: G0463
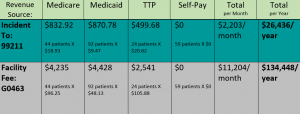
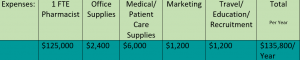
Expenses:
Direct Costs/Revenues
For the first year, the projected net revenue could be anywhere from $26,436 (Incident-To Billing) to $134,448 (Facility Fee Billing), and the projected net expenses are $135,800. If possible, a facility fee would be most lucrative for this clinic. To account for no-shows, we will use approximately a 30% no show rate. Thus, the adjusted revenue would be estimated to be $18,503-$94,113. Using the conservative revenue estimate, the clinic would be about $117,000 short annually in direct costs, and using the facility fee billing, the clinic would be about $42,000 short annually.
Cost Avoidance
However, an important consideration that plays a large factor for this clinic is cost avoidance. There are many different cost avoidance factors that should be taken into account when financial projections are being considered. Some cost avoidance factors include decreasing hospital admissions, decreasing future complications from the disease progression, and decreasing overall medical expenses. For example, annual costs for non-treatment medical expenses are estimated to be $10,500-$148,000 for a liver transplant for a patient with end stage liver disease.1 If we could prevent 10 liver transplants/year, that could easily cover the cost of a pharmacist. Table 1 estimates medical costs associated with Hepatitis C for HCC (hepatocellular carcinoma), DC ( decompensated cirrhosis), and LT (liver transplant).
Table 1:
 (1)
(1)
Studies suggest that patients with chronic hepatitis C who achieve sustained virologic response (SVR) have lower risks of liver-related morbidity and mortality. Table 2 shows the adjusted difference in yearly total mean costs for patients achieving SVR compared to those who do not achieve SVR is $2,648.2 A pharmacist in the clinic could potentially increase the number of patients to achieve SVR by optimizing treatment regimens, educating patients about drug therapy and potential adverse drug reactions, and stressing the importance of strong patient commitment throughout duration of therapy.
Table 2:
 (2)
(2)
Additionally, some interventions made by the pharmacist in the pilot program that provided potential cost savings included performing cost analysis to select the most cost-effective medication, assisting in optimizing a patient’s HCV treatment regimen (medication dosing, selection, titration, ordering), medication screening for drug-induced disease, vaccination recommendations and reconciliations, and insurance inquiry for medication selection or contacting insurance to confirm.3 Because the pharmacist would be removing some of the burden from current practitioners in the Gastroenterology/Hepatology clinic, those providers would be able to see more patients, generating more revenue for Eskenazi Health.
Cost Effectiveness of treatment is also an important consideration. QALY (Quality Adjusted Life Years) can be a way to measure this. These medications are not cheap, but studies have shown that the initial costs of these medications are often worth it in the end. Table 3 summarizes a variety of studies that have shown the cost effectiveness of Hepatitis C medications. For example, Harvoni and Viekira Pak compared to no treatment yields $32,000 to $35,000/QALY, and compared to no treatment, threshold cost for treating F0 with an all oral regimen = $47,000.4
Table 3:
 (4)
(4)
Patient First
Another important factor to keep in mind is the patient’s quality of life. By having access to medications that could cure Hepatitis C, this can tremendously affect the patient’s life in a positive manner.
As the mission of Eskenazi Health is to strive to enhance the ability to meet the needs of the underserved and vulnerable population, this service would be directly aligned with those values.
Break Even
Based upon the estimated financial projections, direct revenues can cover approximately 14% (incident-to billing codes) to 70% (facility fee code) of the total operating costs of the clinic. As previously mentioned, cost avoidance also needs to be factored into the equation. Table 4 estimates the number of interventions needed to cover the remaining costs of the clinic in a year. Realistically, as the number of interventions made by the pharmacist increases, the breakeven point would be approximately 2-3 years. This break even point takes into account both the direct revenue and cost avoidance.
Table 4:

-
Leider AJ, Chesson HW, Xu F, Ward JW, Spradling PR, et al. Cost-effectiveness of hepatitis c treatment for patients in early stages of liver disease. Hepatology. 2015; 61 (6);1860-1869. Doi: 10.1002/hep.27736.
-
Manos MM, Darbinian J, Rubin J, et. al. The effect of hepatitis C treatment response on medical costs: a longitudinal analysis in an integrated care setting. J Manag Care Pharm. 2013;19(6):438-477. doi:10.18553/jmcp.2013.19.6.438.
-
GI clinic interventions, spreadsheet provided by Todd Walroth, PharmD (T. Walroth, electronic communication, February 17, 2017).
-
Graham CS, Greenwald R, Lenz K. Understanding the reimbursement environment in hepatitis c. Centers for Health Law & Policy. http://www.chlpi.org/wp-content/uploads/2014/01/HCV_DPH_Payer_4_5_15_combined_final.pdf. April 2015. Accessed: February 15, 2017.
